The guest blogs from four University of Limerick graduates over the past few weeks have provided fascinating insights into the different stages of training to become a Psychiatrist.
Dr. Diarmuid Boyle focused primarily on starting off in Psychiatry and the Basic Specialist (BST) years:
https://psychiatry7trainingtips.blogspot.com/2020/05/guest-blog-dr-diarmuid-boyle-on-making.html
Dr. Noreen Moloney reflected on those heady days of Higher Specialist Training (HST):
https://psychiatry7trainingtips.blogspot.com/2020/05/guest-blog-dr-noreen-moloney-on-making.html
Then along came Dr. Kevin Lally, who has finished BST and a year as Psychiatry Clinical Tutor in UL and he had a trilogy of blogs on:
Telemedicine and Telepsychiatry: https://psychiatry7trainingtips.blogspot.com/2020/05/guest-blog-part-1-of-dr-kevin-lally.html
and then two blogs on medical education during the COVID-19 pandemic:
https://psychiatry7trainingtips.blogspot.com/2020/06/guest-blog-part-2-of-dr-kevin-lally.html
and
https://psychiatry7trainingtips.blogspot.com/2020/06/guest-blog-part-3-of-dr-kevin-lally.html
Then last week Dr. Frank McKenna, who has also completed BST and a year as Psychiatry Clinical Tutor in UL, reflected on teaching, research and the wide variety of career options within Psychiatry:
https://psychiatry7trainingtips.blogspot.com/2020/06/guest-blog-dr-frank-mckenna-year-in.html
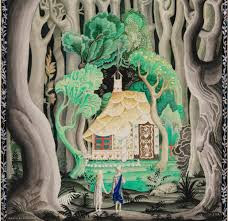
This week I have great pleasure in welcoming Dr. Niall Byrne, yet another extremely bright, energetic and talented graduate of UL who is embarking on a career in Psychiatry while also cultivating a variety of other interests. And this week we are going back to the very beginning of postgraduate training, with Niall's very thoughtful and useful reflections on his Intern year and his hopes and plans for the future. Niall has also included two beautiful works of art to accompany his text.
So thank you Niall and it's over to you...
Dr. Niall Byrne - biography
I am to commence the Psychiatry Basic Specialist Training (BST) sceheme in Dublin in July, after completing the academic internship at Galway University Hospital. I graduated from the Graduate Entry Medicine programme at the University of Limerick in 2019. I am interested in innovation in medicine and research and hope to specialise in Child and Adolescent Psychiatry. Beyond this I am interested in art and videomaking and I have recently made comedy medical voice over videos which has been circulated among the medical community across the country: https://www.instagram.com/medhumer/?hl=en
Reflections
As I reflect upon the past 12 months, I feel a sense of achievement
having overcome the steepest learning curve of my life, but I am apprehensive for
changeover. I was fortunate enough to achieve the only academic internship post
to include a psychiatry rotation, which was based entirely in Galway University
Hospital (GUH). My first three months were in general adult psychiatry and I
was based mainly in the acute Mental Health Unit (MHU), which is an impressive
two-storied newly built facility with over 50 in-patient beds.
I was split between two consultants and worked on the community
mental health (CMH) team under Dr Brian Hallahan, attending weekly multidisciplinary team meetings as well
as outpatient clinics. The CMH multi-disciplinary team understood the patient’s
life beyond their diagnosis, something which is not afforded the same amount of
discussion in other specialties, which is essential to that patient’s
management. Moreover, I found out-patient clinics a particularly helpful means
in developing my clinical acumen. As my confidence and knowledge base developed,
I was seeing patients alone and making decisions and changes to patient’s
management.
On Professor Colm McDonald’s team, we looked after the acute adult
in-patients. I was given the opportunity to present case discussions and do
full medication reviews as well as attend rounds and making adjustments to
inpatient’s medical management where necessary. My perceptions of
psychiatry practice prior to working quickly transitioned into reality and I
was relieved by how much it lived up to my expectations. On one occasion I
presented a complex case of refractory paranoid schizophrenia during the weekly
case presentations, and together we devised a treatment plan. This was a
rewarding experience. As a psychiatry intern, you get as much out of it as you
invest. You can have minimal responsibility, or you can really get enthralled
and maximize your learning. I tried to gain as much as possible as I was
strongly leaning towards a career in this field for a number of years.
Rainy Day by Phan Tru Trang
The one major setback to commencing the intern year on a psychiatry
rotation is having to do medical call with minimal exposure to acute medicine during
the day job. When starting off on my extended days even navigating around the main
hospital was challenging. On one of my first nights the medical registrar
questioned why a psychiatry intern was doing medical call, when we both had to
manage a deteriorating patient on one of the wards. However, he later
apologized for the comment and admitted that he was stressed because it was his
first day in GUH. I quickly learned that if people are difficult there is
generally an underlying reason and you just have to give them the benefit of
the doubt and not let it affect your own performance. Although if it is
something more persistent or it hinders your patient’s care then it should be
dealt with appropriately to avoid conflict, burnout or mismanagement.
After psychiatry I rotated onto vascular and general surgery. I enjoyed the level of responsibility being on such a small team. Surprisingly, there were several opportunities to develop my psychiatry skills. One episode that stands out was a middle-aged female patient who was admitted with painless jaundice. She needed a CT and my registrar informed me that she was 'too nervous' to go through with the scan. I insisted on carrying out a brief psychiatric assessment which revealed a long-standing history of generalized anxiety with progressive loss of function that was refractory to treatment. She also suffered a number of traumatic life events that she had not disclosed previously. I arranged for a liaison psychiatry review and she was commenced on treatment and would be followed up in the community. I taught her some basic mindfulness and prescribed a stat dose of alprazolam. She completed her scan and was discharged. She said this experience had saved her life and would make a great change going forward; she was so grateful that she gifted me with an angel statue during a follow up appointment.
My current rotation is in respiratory
medicine, which brings with it a heavy workload, but the team were particularly
easy to get on with and made the experience much more enjoyable. I found myself
enjoying medicine a lot more than I anticipated and was particularly fond of
acute management while on-call. Eventually I was making medical decisions on-call
and during the daytime with confidence and my procedural and management skills
developed rapidly.
When the COVID pandemic emerged, my team
was at the forefront. However, I remained the only intern on the wards which
brought with it additional responsibility. The respiratory inpatients at this time
were highly specialized cases, mainly patients with cancer and cystic fibrosis.
For a long period of time it was just me, the consultant and an SHO. I was arranging
family meetings and breaking bad news to patients and families, which although
was difficult, it was a great learning opportunity. As an intern we have the privilege
of being able to re-visit patients who may have received bad news on a round or
who don’t quite understand their management regimen, etc. Something I carry into
my career was said to me by a dear friend of mine, who told me that when her
mother, who is a nurse and suffered from acute leukaemia, said that sometimes
all she needed was for someone that she can vent with. I would always take the
time to see patients later on in the day and give them the time they needed, to
explain or to simply lend an ear from person to person. In medicine there’s a
tendency to launch towards a psychiatry referral for someone going through an
acute adjustment reaction or who has psychosocial stressors without even
enquiring about a psychiatric illness. I think offering these patients a
psychiatry referral is insulting to both the patient, and the speciality, and
it is a message I always stress, to avoid this from happening. A patient should
not be labelled as requiring psychiatry input for experiencing human emotion.
Every
intern will encounter a trauma or case that will affect them. Our resilience
can only be stretched so far. GUH’s cohort of interns and staff in general are
kind and willing to help one another and this sense of comradery softens the
blow of the intensity of the intern role, a role which is diverse, challenging
but rewarding. I am happy to say that I thoroughly enjoyed my job and found the
year rewarding and eye opening.
I will
commence the Psychiatry BST as an SHO as part of the UCD deanery in mid-July. I
have mixed feelings as I have fallen in love with Galway and GUH and will miss
it and many people dearly. At the same I am excited to begin my training as a
psychiatrist, and I am confident that this is the right path for me having
reflected upon my experiences. My goals are to bring about change for patients
and for colleagues. As I specialize in this field, I will dedicate time to
quality assurance, research and education. Most importantly I will carry the
message to be kind to your colleagues and to always be an advocate for your
patients.
After
the Rain by Phan Tru Trang